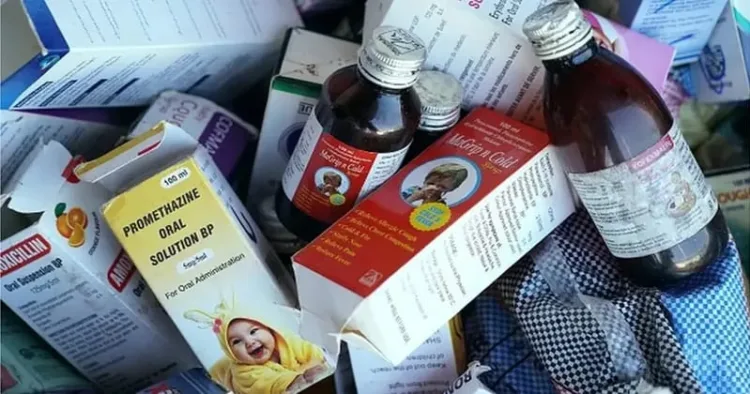
The latest cough syrup catastrophe prompted the investigation, which points to institutional flaws: dozens of incidents of phoney or contaminated drugs were discovered between 2023 and 2025, but the majority of offenders received little to no penalty. Gujarat government authorities discovered a factory in Kutch producing fake Colgate toothpaste using “cheap and substandard” components, along with phoney Sensodyne, Eno, and cigarettes. In August 2025, the Uttar Pradesh Food Safety & Drugs Department and STF Special Task Force conducted raids on stores in Agra and Lucknow, confiscating more than Rs 200 crore worth of counterfeit medications and apprehending several vendors. The network was importing fake medications from Chennai and Puducherry and marketing them as well-known brands for diabetes, pain management, colds, and coughs. One trader from Agra was apprehended during these raids, offering Rs 1 crore in cash bribes to delay the probe.
Over the course of a 60-hour operation, police in Kanpur discovered two illegal factories manufacturing 434 different kinds of counterfeit medications, valued at approximately Rs 4.5 crore. Using intricate computer records, the defendants sold these tablets all over India, including to Africa and Afghanistan, in order to evade detection.
Reports of negative patient reactions have worried Punjab officials elsewhere in north India. Eight intravenous fluids and injections, including batches of normal saline, dextrose 5 per cent, ciprofloxacin, and a bupivacaine–dextrose mix, were banned by the Health Department in mid-October 2025 after dozens of patients became ill. All hospitals were instructed by a government circular to immediately stop using the questionable batches while tests were conducted. Products from well-known firms were impacted by the recall, which prompted Punjab’s health minister to launch an investigation and vow to take action against any dishonest suppliers.
The medicines regulator in Rajasthan also discovered a pervasive issue. Hundreds of prescription samples in the state, including necessary antibiotics (such as amoxicillin and ciprofloxacin), antihistamines, diabetic medications, and painkillers, failed quality testing, according to an India Today investigation published in October 2025. It is concerning that a large number of these counterfeit or inferior medications were already on store shelves and administered to patients prior to being reported.
Lethal health risks of counterfeits
These counterfeit goods have the potential to be fatal in addition to being scams. Experts caution that hazardous alternatives or incorrect dosages are frequently found in counterfeit medications. For instance, counterfeit antacid powders (such as Eno) may include dangerous ingredients that cause allergic reactions, bleeding, or stomach ulcers. False antibiotics and pain relievers could include harmful adulterants or no active substance, leaving infections and inflammation untreated and perhaps leading to organ damage. The counterfeit commonplace products are “slow poisons”; for example, tainted toothpaste can damage teeth and gums, phoney smokes might contain harmful mixtures, and even tainted instant masalas can include carcinogens.
The report from Rajasthan is terrifying: hundreds of children may unintentionally take fake medications before authorities discover the batches are faulty. Such fake medications have previously killed people overseas; in 2022, cough syrups made in India killed 70 children in the Gambia and 19 in Uzbekistan, raising panic throughout the world. When patients were unwell earlier this year, Punjab in India also had to recall Ringer’s lactate and regular saline. Doctors in Punjab complain that “patient care goes for a toss if we can’t ensure the quality of basic IV fluids.”
How to spot fakes and stay safe
Customers need to be on the lookout. Steer clear of offers that look too good to be true and only purchase medications from authorised pharmacies and trustworthy internet vendors. Examine the container carefully because authentic medications often have a scratch-off panel or QR code for authentication, along with batch numbers and expiration dates. Regulatory authorities caution against trusting unsourced products and suggest checking for strange packaging or spelling mistakes. Always “buy products from authorised sellers and verify packaging details for authenticity before use,” as one official stated.
Look for certified logos and complete manufacturer data for common products like toothpaste or masalas. Notify local drug regulators or consumer helplines if you come across questionable products. (Hotlines for consumer complaints have been established by authorities in Haryana and other states.) Demand medications from hospital stock (which should be quality-checked) in medical crises, and if you are unsure of the source, ask chemists.
Government response and policy measures
Authorities have tightened enforcement as a result of these instances. As part of a fresh crackdown, the Union Health Ministry has revoked and suspended the licenses of numerous negligent pharmaceutical manufacturers. Mansukh Mandaviya, the health minister, declared in March 2023 that companies producing fake medications “will not be spared.” Particularly after the WHO connected Indian cough syrups to infant fatalities, the government even set aside more funds (about $80 million) to improve drug regulatory labs and inspections across the country.
New rules are on the horizon, according to officials. The Central Drugs Standard Control Organisation (CDSCO) is getting ready to impose legal responsibility on distributors and merchants for the first time. A proposal being considered in drug consultative meetings would penalise chemists and distributors for simply storing or selling counterfeit medications, closing a loophole that currently protects them as long as their invoices seem legitimate. Essentially, each supply chain link would need to demonstrate quality monitoring, or risk prosecution. Stricter sourcing regulations are also being considered by the government; for instance, pharmacies that purchase from odd out-of-state vendors, which is a known indicator of illegal supply, may be flagged.
Other recommendations include- Mandate unique, scannable QR codes on all packaged medicines—especially antibiotics and syrups—linking to a central registry so consumers, doctors, pharmacists and regulators can verify authenticity instantly. Require pharmaceutical companies, importers and manufacturers to print codes on primary and secondary packaging, and oblige chemists and hospitals to scan on receipt. Expand accredited drug-testing capacity with additional fixed and mobile labs to clear seizure backlogs, prioritising rural districts. Classify deliberate mislabelling or shady sales as non-bailable offences with custodial sentences for owners and complicit chemists. Strengthen pharmacovigilance so adverse-reaction signals automatically trigger rapid batch investigations and field inspections. Coordinate implementation through government ministries in consultation with the IMA and professional bodies to align clinical guidance, supply-chain oversight and enforcement, benefiting patients and consumers. Doctors should source medicines from accredited suppliers, prescribe clearly (prefer generic names), and record brand, batch, expiry and QR/barcode details in the medical record. For high-risk drugs, staff should scan and verify packaging, counsel patients on authenticity checks, and prefer e-prescriptions linked to pharmacies. Adopt antibiotic-stewardship principles to reduce unnecessary use. If packaging appears suspicious, quarantine the batch, retain samples, and report immediately to the hospital pharmacy, pharmacovigilance unit and drug authorities. Train junior staff on inspection, documentation and escalation procedures to ensure rapid detection, investigation and patient safety. This protects patients and strengthens supply-chain accountability nationwide, urgently and transparently.
Public awareness campaigns: Use television and social media to begin educating the public about fake “online pharmacies” and home delivery services that don’t require a prescription.
It is necessary to improve the collaboration between customs, police, and narcotics authorities. As demonstrated in the situations of Punjab and the Gambia, a large number of counterfeit medications enter through interstate or cross-border networks. These rings can be broken up more successfully by exchanging intelligence and conducting raids together (as demonstrated by the recent joint STF-drug department actions in UP).
The severity of India’s counterfeiting issue is demonstrated by the latest wave of phoney drug busts. Every time inferior medications make their way into the market, thousands of lives are at risk. The public has been outraged by consumer goods scandals (masala, phoney toothpaste), but contaminated medical supplies can be even more deadly. Experts caution that counterfeit medications will continue to circulate “under the radar” unless severe sanctions and thorough inspections are swiftly implemented. The good news is that authorities are finally taking action: raids are getting more frequent and new legislation is being developed. However, in order to eradicate toxic counterfeits from Indian pharmacies, authorities must maintain their vigilance and consumers must remain vigilant. Patients can then be guaranteed that the medication they purchase is safe, authentic, and not a lethal imposter.
India has become a global hub for healthcare solutions, drawing medical tourists from all over the world with its reasonably priced medications, vaccines, and specialised therapies. This reputation is supported by its robust pharmaceutical manufacturing base, highly qualified physicians, and growing research infrastructure. But with fame comes responsibility: authorities, producers, and suppliers need to be on the lookout for fake medications, poor quality, and weaknesses in the supply chain. To safeguard patients and maintain trust, testing capacity should be strengthened, serialisation should be enforced, and transparent verification should be encouraged. India can maintain its promise of health tourism and keep providing safe, high-quality pharmaceuticals and vaccines to patients both domestically and abroad by fusing innovation with strict control and patient-centered standards.













Comments