Leprosy or Hansen’s disease, once carried a weight of fear and stigma across India is now fading at a fast pace. It is a chronic infectious disease caused by Mycobacterium leprae which affects the nerves, respiratory tract, skin and eyes. Its early signs include discoloured skin patches, loss of sensation to touch, pressure, pain or temperature, muscle weakness, ulcers that fail to heal with deformities in hands, feet and face. In severe cases patients may lose the ability to close their eyes, leading to poor vision. Spread through droplets from the nose and mouth during close and frequent contact with untreated cases, the disease was long feared because of the deformities it has created the root of deep social stigma.
Leprosy appears in two forms, first is multibacillary, showing a high density of bacilli on slit-skin smear examination and second is paucibacillary with few or no bacilli visible. The revolution in its treatment came in 1983 with the introduction of Multidrug Therapy (MDT), a combination therapy recommended by the World Health Organization (WHO) and was provided free of cost to all patients. MDT not only halted transmission but also prevented disabilities and deformities when given early. After its introduction, India has seen a remarkable fall in incidence and prevalence rates.
From Control to Eradication: The Early Years
India’s battle against leprosy started within a short while after Independence. The Census of 1951 had reported 13,74,000 cases of leprosy with a prevalence rate of 38.1 per 10,000 population. Realizing the magnitude of the problem, the Government of India initiated the National Leprosy Control Programme (NLCP) in 1954–55. During the Fourth Five-Year Plan (1969–1974) it became a centrally sponsored programme, gaining momentum and funding support.
To widen its reach NGOs were brought into the framework through the Survey, Education and Treatment (SET) scheme in 1983. SET was deployed in moderate and low endemic areas and urban leprosy centres in cities, became the nerve centres of the control drive. Each sector of 25,000 population was assigned a paramedical worker, supervised by a non-medical officer for every five workers. These groups were supposed to make house-to-house visits in two-years, making diagnosis by slit-smear methods and giving treatment that occasionally went on for more than a decade.
The treatment power relied on its community link and counselling was provided to patients at village clinics and they were encouraged to bring relatives with them, reducing stigma and awareness. Health education came to be at the center of all activities, initiating India’s Information, Education and Communication (IEC) strategy in leprosy control. Treatment began with Dapsone monotherapy, which was later replaced by MDT recommended by WHO in 1982 which consists of bactericidal Rifampicin and bacteriostatic Clofazimine.
This shift in 1983 marked the birth of the National Leprosy Eradication Programme (NLEP), embodying vision of compassion and inclusion for those afflicted. From the beginning, India’s strategy focused not only on cure but also on restoring dignity through early detection and free treatment.
The National Mission for Elimination
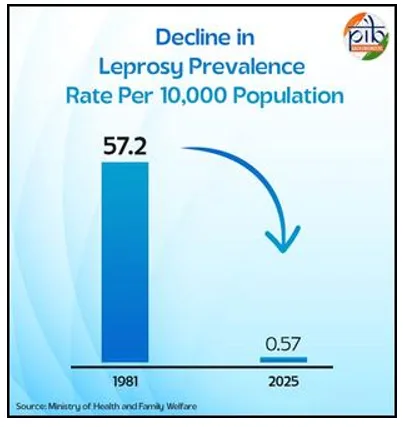
The NLEP functions under the National Health Mission (NHM), a three-layered strategy with political will, decentralised delivery and public awareness. Prevalence of leprosy declined from 57.2 per 10,000 between 1981-2004 to merely 2.4 per 10,000. The percentage of patients with obvious deformities (Grade II disability) fell from 20 per cent in 1981 to 1.5 per cent in 2004.
The World Bank supported two major projects (1993–2000 and 2001–2004), were supported by the World Bank with a focus on community involvement and IEC innovations. Collaborations with WHO and mass media organizations such as BBC World Service Trust and Lintas enhanced outreach of SOMAC. Special attention was given to women, tribal communities and urban poor. Integration with the general health system empowered Auxiliary Nurse Midwives (ANMs) and Anganwadi Workers (AWWs) to participate actively.
By March 2004, 17 states and 250 districts had achieved elimination, defined as less than one case per 10,000 population, while seven more were close to the goal. India achieved national elimination in December 2005.
Strategies That Changed the Course of treatment in 2025
NLEP integrated response includes free diagnosis and MDT treatment for all patients, along with Post Exposure Prophylaxis (PEP) using single-dose Rifampicin for healthy contacts. In 2025 a new triple-drug regimen was available for both Paucibacillary (PB) and Multibacillary (MB) cases.
For early detection of cases, several campaigns are at work:
- Leprosy Case Detection Campaign (LCDC) is door-to-door surveys in high-endemic settings.
- Focused Leprosy Campaigns searches in villages where Grade II disability or child cases are seen.
- Special Plans for hard-to-reach populations.
- Healthy Contact Examinations and Retrospective Contact Tracing for the last five years.
- ASHA-Based Surveillance for Leprosy Suspects (ABSULE) for low-endemic areas.
Beyond detection the Disability Prevention and Medical Rehabilitation (DPMR) scheme offers education, counselling, Micro Cellular Rubber (MCR) footwear, self-care kits, aids like splints and crutches other reconstructive surgeries are offered. Patients are given Rs 12,000 compensation for loss of wages for surgeries.
Building capacity continues through regular training of physicians, laboratory technicians, physiotherapists, supervisors of health and ASHAs. Periodic awareness campaigns like Sparsh Leprosy Awareness Campaign are organized around Anti-Leprosy Day every year which decreases stigma and promotes voluntary reporting.
NLEP has also advocated scrapping discriminatory leprosy laws and enhancing surveillance. From 2025, all sectors of the health system such as government, private, NGO and medical colleges are required to report cases of leprosy. The ASHA-Based Surveillance for Leprosy Suspects (ABSULS) program intensified case detection at the grassroot level. Digitalization via Nikusth 2.0, introduced in 2023 streamlined record-keeping, drug stock management and patient tracking.
The National Strategic Plan (2023–2027): Roadmap for Zero Transmission
According to the Global Leprosy Strategy 2021–2030 and WHO’s Roadmap for Neglected Tropical Diseases, India’s National Strategic Plan (NSP) 2023–2027 targets interrupting transmission by 2030. It emphasizes targeted detection, new diagnostic tools, chemoprophylaxis, antimicrobial resistance surveillance and post-treatment care.
Key focus areas include where focus is made:
- Accelerated new case detection.
- Advanced digital surveillance.
- Introduction of new safe vaccines.
- Strengthened post-cure care and rehabilitation.
- Sustaining expertise and integrating multi-disease services.
- Impactful behavioural change communication.
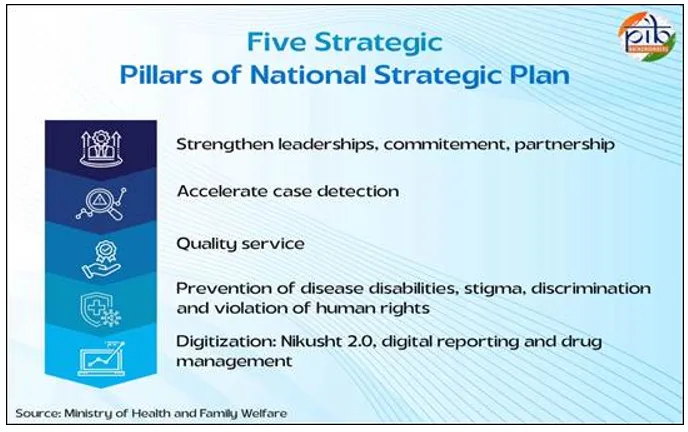
The Plan envisions district-level interruption of transmission, evidenced by zero child cases for five consecutive years, followed by full elimination when no new cases appear for three years. This mission is powered by a whole-of-government and whole-of-society approach, leveraging technology, inter-departmental coordination and civil participation.
India’s comprehensive framework for elimination includes:
- Integration with Ayushman Bharat Yojana for leprosy screening for all individuals above 30 years of age.
- Integration with Rashtriya Bal Swasthya Karyakram (RBSK) and Rashtriya Kishor Swasthya Karyakram (RKSK) for screening of children aged 0–18 years.
- DPMR Services for reaction management, MCR footwear, aids and appliances and self-care kits.
- Nikusth 2.0 ICT Portal was launched on January 30, 2023 by the union Health minister to track diagnosis, treatment and follow-up.
- National Anti-Microbial Resistance Surveillance Guidelines were launched the same year to monitor resistant leprosy strains.
- National Framework for Mental Health Integration helps in addressing psychological aspects for patients and families.
- Revised Treatment Regimens (2025) attached new classification for PB and MB cases effective from April 1, 2025.
- PVTG Tagging System within Nikusth 2.0 for 17 states with Particularly Vulnerable Tribal Groups under PM-JANMAN.
- Special Monitoring for 121 districts with prevalence above one per 10,000 population, focusing on high child and disability rates.
As of March 2025, 31 states and 638 districts record prevalence below one case per 10,000 people. The prevalence rate has fallen from 57.2 per 10,000 in 1981 to just 0.57 in 2024–25. New case detection declined from 9.73 per 100,000 (2014–15) to 7.0 (2024–25). Child cases dropped from 9.04 per cent to 4.68 per cent in the same period, reflecting reduced transmission. Grade 2 disability declined from 4.68 to 1.88 per million showing early detection success.
Post Exposure Prophylaxis (PEP-SDR) coverage among eligible contacts increased from 71 per cent in 2019–20 to 92 per cent in 2024–25. The Leprosy Case Detection Campaign confirmed 27,428 new cases in 2024–25 thus ensuring timely treatment and surveillance. Integration with RBSK, RKSK and Ayushman Bharat has enabled age-inclusive screening across the country.
Global Partnerships and Recognition
India’s collaboration with the WHO has been crucial for free MDT supply, technical guidance and independent evaluation. In the World Health Assembly of 1991, India reaffirmed its commitment to elimination. Though the national goal was achieved in 2005, India efforts continued with renewed focus. WHO supported India Modified Leprosy Elimination Campaigns (MLECs), diagnostic improvements and Special Action Projects for hard-to-reach populations.
The COMBI (Communication for Behavioural Impact) strategy, piloted in Bihar has changed community perception about leprosy. India also contributes to global leprosy policy through the Global Leprosy Strategy and The Global Appeal (since 2006), advocating against discrimination.
Partnerships with the International Federation of Anti-Leprosy Associations (ILEP), Sasakawa Health Foundation, World Bank, Global Partnership for Zero Leprosy (GPZL), Hind Kushth Nivaran Sangh, ALERT India, IAL, IADVL, BLP, Schieffelin Institute Karigiri and International Leprosy Union have further strengthened India’s outreach and rehabilitation initiatives. In 2023, WHO acknowledged India sustained success since 2005, highlighting it as a model for integrated public health management.
Journey of Commitment and Compassion
From 39.19 lakh patients under treatment in 1981 to just 0.82 lakh in 2025, India has achieved a 98 per cent drop in caseload and 99 per cent fall in prevalence. New case detection has fallen by 37 per cent since 2006.
This success is support of government, free and uninterrupted MDT supply, partner support, decentralised implementation and strong community engagement. The NLEP has transitioned from a vertical to integrated service delivery model, combining digital surveillance, innovation and preventive care.
It’s a saying that elimination is not eradication. New cases may still emerge. The goal now is interruption of transmission detecting cases early enough to prevent disabilities and ensure no child suffers from leprosy again.
The government continues to strengthen surveillance, awareness, and capacity-building, focusing on rural and tribal communities. With digital tools like Nikusth 2.0, proactive PEP coverage and the National Strategic Plan 2023–2027, India is advancing toward a leprosy-free future by 2030.
As the nation is ready for eradication achievement, the journey of leprosy control becomes more than a health success but it is a story of resilience, empathy and collective human progress.


















Comments